Thanks to @aga.ayush11, have been doing more groundwork on Krsnaa with him.
Sharing high level takeaways from a call with an industry expert.
Context: They are a low cost diagnostics company, they participate in PPP
tenders where the group overall has 80 Cr. of revenue. They have around 20 years
of experience in the diagnostic industry, and have gone head to head with Krsnaa in the past.
On the PPP landscape in India
-
PPP in India has seen huge success in the last 5 years, currently it is in a
growth phase that will last for 10-15 years. It is not nascent, and is not yet
mature. -
There are two drivers of growth:
- So far PPP tenders have been in radiology, increasingly, tenders in pathology
are being rolled out. The next gen of PPP tenders will be in mammography,
dialysis, etc. - The size of these tenders is now growing as states have finished one iteration
(generation 1) of PPP tenders from 5-10 years ago.
Governments start by rolling these out in medical colleges → super speciality hospitals → district and sub-district hospitals.Generation 2 tenders are larger as evidenced in Rajasthan. Any large player who wins these can grow at 30-40% CAGR for the next 6-7 years unsurprisingly.
- So far PPP tenders have been in radiology, increasingly, tenders in pathology
-
For example, West Bengal alone has a 1000 Cr. of PPP diagnostics market size per year. Larger
states have a market size of 2000 Cr. +. Overall market landscape in India today is probably close to 15 – 20,000 Cr. -
States can choose to do in-house, or go down the PPP route. Eventually, more states will do PPP.
On the nuances of tender bidding
-
The authorities that float the tender, and the authority that carries out the day
to day operations are two completely different bodies. -
The largest challenge currently in PPP tenders is meeting the technical
criteria. This is a significant barrier to entry. Governments have stopped
floating tenders where you do not need experience. Now you need 3+ years
of MRI experience under PPP. New players get stuck here. You may have
resources and funding, but meeting experience criteria is tough. Even if you
choose to make a consortium with someone else, governments have killed
consortiums by saying leading players need experience. -
There is no chance to influence the outcome of a tender in any way. These are carried out in a transparent manner.
-
Tenders are awarded on largest discount to CGHS rates. CGHS for MRI is
2000 rupees, but you have 40 different MRI tests benchmarked to this rate.
Different body parts, contrast, etc. The weighted average of these 40 tests on
a CGHS rate of 2000 actually comes out to 3000 rupees. -
The unit economics can be vastly different depending on the type of hospital. If it is a medical college, one can expect higher number of scans per day. If it is a super speciality hospital, the test mix will be different. The game in bidding for a tender is to think about what test mix one expects, and bid accordingly.
Working with the government, and receivables
-
Budget for National Health Mission is given by the centre. The states where centre + state
have the same party in power, adoption of PPP is not a challenge. For other states like Punjab or West Bengal, state governments try to portray the scheme as theirs, not the centre’s. State-centre politics play a large role in successful PPP adoption. -
We have never had to write off any receivables. Governments have a healthcare budget and have to make sure budget spend is accounted for, so receivables is not a problem.
-
The largest external driver of how quick receivables comes to you is whether
the centre + state have the same ruling party. Centre wants very specific data
for PPP tests: 1. Sex of patient, 2. Age, 3. Name, 4. Condition. If centre and
state are the same party, this is done quickly.
Operational Highlights
-
There are two kinds of implementations of PPP: citizens pay at a discount to CGHS rates, and free diagnostics initiative. Ultimately, even if tests are life or death, someone who doesn’t have purchasing power will think 20 times before getting a 2000 rupee test done. For this reason, scaling centres is much faster when this is done via free diagnostics.
-
More states are going down the free route as it gives you immense political capital to pitch free diagnostics to your citizens.
-
Private walk-ins is a very reasonable model to target for someone like Krsnaa. OPD patients are all seen by 5pm, and as long as you prioritise hospital clients first, no one objects to private walk ins. 5pm – 11pm is a great time for this.
-
Awareness of free diagnostics is a critical theme. We’ve seen in our state that it took 3-4 years from the centre starting to seeing peak footfalls.
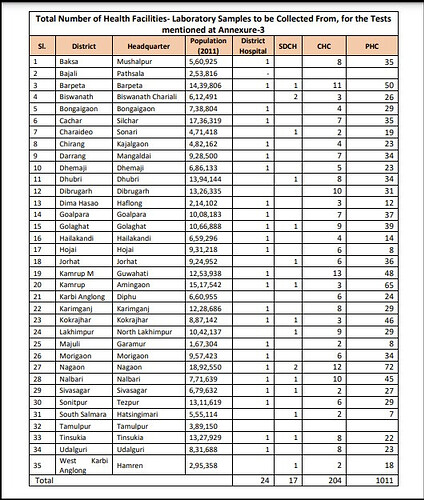
PS: there are a couple of large tenders currently being floated by governments. One closing in a week is a statewide pathology tender in Assam:
Disclosure: Invested, in top 5 positions, transactions in the last 30 days.
| Subscribe To Our Free Newsletter |